
Close
Enquiry
Please see contact information below or complete the form and we will get in touch with you.

Parsons Green
3rd Floor Brigade House
8 Parsons Green
London
SW6 4TN
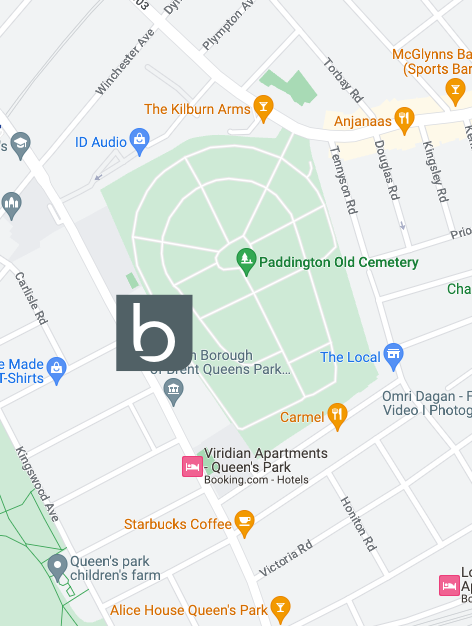
Queen's Park
2nd Floor
105-109 Salusbury Road
London
NW6 6RG

Jesse's House
8-10 Heathmans Road
Parsons Green
London
SW6 4TJ
COVID-19 Safeguarding & Operational Policy
BEYOND HEALTH COVID-19 SAFEGUARDING & OPERATIONAL POLICY
version 3.0, 01/02/2022
Please note: Evidence for COVID-19 is changing frequently. This document will be updated as often as possible. Staff will be required to conduct any necessary training as a consequence of any updates made.
Key Messages
1. We work within the legal, regulatory and professional frameworks that guide the safe management of patients, the safety of the wider public and everyone who works in the practice environment for which we are responsible.
2. We follow Public Health England (PHE) COVID-19 infection prevention and control (IPC) guidelines.
3. A full risk assessment of the working environment for which we are responsible has been undertaken and documented which demonstrates that all measures designed to mitigate risk and fulfill our legal and regulatory obligations are in place.
4. We provide and use appropriate personal protective equipment (PPE) and have systems and policies in place that govern its use.
5. We have a ‘virtual first’ approach where-by remote consultations remain standard practice during this period and we undertake per patient risk assessments to make a clinically reasoned decision for offering either a face-to-face or remote consultation for each patient and for each of their planned contacts. We document our rationale for these decisions.
6. We engage in discussions regarding the rationale for remote or face-to-face consultations with the patients. Face-to-face consultations only occur If both parties deem it necessary to proceed with face-to-face care. The patient is made aware of all current risks associated with this approach and they provide consent in advance of the face-to-face consultation.
7. We demonstrate our duty of care as employers by ensuring all staff are trained and competent in the procedures necessary for the safeguarding of patients, employees and the general public during the covid-19 pandemic.
1. Legal, regulatory and professional responsibilities
We work within the legal, regulatory and professional frameworks that guide the safe management of patients, the safety of the wider public and everyone who works in the practice environment for which we are responsible.
All registered healthcare practitioners regardless of profession, sector or setting owe a duty of care to their patients.
We have a duty of care to provide a reasonable standard of care to patients and to act in ways that protect their safety and uphold the statutory standards for UK-wide registration as dictated by The Chartered Society of Physiotherapy (CSP) and the The General Osteopathic Council (GOsC).
We must also comply with the Health and Care Professions Council (HCPC):
Specifically, the following apply:
- 6.1 You must take all reasonable steps to reduce the risk of harm to service users, carers and colleagues as far as possible.
- 6.2 You must not do anything or allow someone else to do anything which could put the health or safety of a service user, carer or colleague at unacceptable risk.
- 15.1 Understand the need to maintain the safety of both service users and those involved in their care.
- 15.3 Be aware of applicable health and safety legislation, and any relevant safety policies and procedures in force at the workplace, such as incident reporting and be able to act in accordance with these.
- 15.4 Be able to work safely including being able to select appropriate hazard control and risk management, reduction or elimination techniques in a safe manner and in accordance with health and safety legislation.
- 15.6 Be able to establish safe environments for practice which minimise risk to service users, those treating them, and others, including the use of hazard control and particularly infection control
In the context of COVID-19, these responsibilities extend to:
- Complying with government social distancing and shielding directives and mitigate as far as reasonably practicable the risk of transmitting the disease to patients and the wider general public, particularly to those in the vulnerable and extremely vulnerable categories.
- Using appropriate personal protective equipment and manage any clinical areas in accordance with COVID-19 infection prevention and control regulation
2. Infection prevention and control (IPC) measures
We ensure we have all appropriate systems and processes in place to comply with government guidance on Infection prevention and control (IPC) measures
We follow up to date government guidance on infection prevention and control measures
We have conducted mock patient and staff journeys throughout the clinic to assess what they may touch or be exposed to and also consider how social distancing could be maintained in the common areas. This has enabled us to conduct a risk assessment and introduce the risk mitigation strategies discussed below.
3. Risk Assessment of the environment for which we are responsible
A full risk assessment of the environment for which we are responsible has been undertaken and documented which demonstrates that all measures designed to mitigate risk and fulfill legal and regulatory obligations are in place.
The following guidance has been followed to undertake the risk assessment of your clinic environment and put in place mitigating actions to manage risks:
- government social distancing directives
- government IPC guidance
- additional information from the Health and Safety Executive
- government advice on working safely during COVID-19
The following risks and mitigation strategies have been identified and put in place:
- Risk of transmission between any persons within the building
Mitigation strategies:
- reduced clinic capacity to limit number of people within the building at any one time and to ensure any patients attending can be kept 2m apart
- maximum of 4 (2 clinicians and 2 patients) at any time in the rehabilitation gym space
- Risk of transmission by incoming clients
Mitigation strategies:
- screening patients for personal &/or household COVID symptoms or exposure within 14 days &/or vulnerability prior to appointment
- addressed within prescreening questionnaire conducted by CST at time of booking
- requirements to disclose / not attend covered in appointment reminder text/email 48 hours prior to appointment
- addressed during triage by Clinical team prior to confirming face-to-face appointment appropriate and justified
- requirements for incoming clients
- wear a face mask whilst in clinic (on site masks available in the instance this is not respected. Client Services Team (CST) to notify clients of requirement and request this is respected at any subsequent visits) and to be dressed in appropriate clothing for their session
- wear the clothing they will be wearing during their treatment session (to reduce movement in building and clothing left on surfaces during treatment)
- arrive on time
- sanitize hands upon entry to and exit from clinic (hand washing/sanitizing posters and PHE hand wash/sanitizers located in lower hall, reception, bathroom and gym space)
- requirements explained by CST at time of booking and included in email communications
- other
- other
- clinic to operate a cash free policy and as a preference client payment taken online
- magazines and fruit bowls removed from reception
- clinical staff to consider adaptations or alternatives to treatment techniques to reduce proximity
- public health information displayed at entry to clinic, in reception and in bathrooms
- Risk of transmission by staff
Mitigation strategies:
- COVID-19 training to be completed prior to return from furlough and at time any new updates made refer Appendix 4
- All staff to sanitize hands upon entry to and exit from clinic and prior to and after all treatment sessions
- All staff to have temperature check performed upon arrival (using infrared medical temperature gun)
- Requirement to wear face mask at all times whilst in clinic
- Staff assigned a fixed room rather than using multiple spaces
- PPE to be worn and taken on/off inline with Beyond Health COVID-19 Safeguarding & Operational Policy and applicable govt./regulatory requirements
- Process for safe disposal of PPE to be followed inline with Beyond Health face-to-face guidance document and applicable govt./regulatory requirements
- Staff asked to refrain from using public transport for travel to and from work
- Risk of transmission within the building (surfaces, other)
Mitigation strategies:
- Reception and treatment room windows to remain open when reasonable to do so during hours of operation to ensure good ventilation
- Doors to be left open where possible to reduce touch points
- Increased cleaning by vendors refer COVID 19 Cleaning Policy – Appendix 4
- High touch surfaces identified and cleaning timetable established to ensure more frequent and thorough cleaning throughout open hours refer COVID 19 Cleaning Policy – Appendix 4
- Paper sheets used in place of bed covers and over pillows/head rests
- Door to adjacent GP locked and staffroom has been moved to treatment room 3
- Dry-cleaning to be exchanged at front door
- PPE and cleaning procurement plan for 12 months to ensure adequate supply
4. Personal Protective Equipment (PPE)
We provide and use appropriately PPE and have systems and policies in place that govern its use.
We follow up to date government guidance on PPE for use in NHS and social care settings. This guidance has been used to inform the use of PPE for healthcare professions operating in the private health sectors.
We also follow the guidance from the Chartered Society of Physiotherapy.
Clinical staff are required to wear the following:
- Single use nitrate gloves
- Single use plastic apron
- Fluid resistant surgical masks (FRSM Type IIR). If these are not available a Filtering Face Piece Respirator FFP2 or Filtering Face Piece Respirator FFP3/KF99 may be used
Client Services staff are required to wear the following:
- Fluid resistant surgical masks (FRSM Type IIR). If these are not available a Filtering Face Piece Respirator FFP2 or Filtering Face Piece Respirator FFP3/KF99 may be used
The maximum time a mask and apron may be worn is 4 hours or when the clinician leaves the care setting/exposure environment. Masks must also be replaced if:
- Dirty or contaminated
- Damaged
- Damp
- It is difficult to breathe through or uncomfortable
Single use nitrate gloves and aprons must be removed and replaced immediately after each treatment session or when the clinician leaves the care setting/exposure environment if this occurs during the treatment session.
Face-to-face contact will not proceed unless the appropriate PPE is available.
PPE must be put on and removed correctly. All staff are required to train in and follow the guidelines of the WHO: COVID-19: How to put on and remove personal protective equipment.
PPE is stored in a clean/dry area until required for use and expiry dates are adhered to.
PPE is disposed of in a specific waste bin separate from clinic normal waste. It is labeled with the date of seal and put aside for 72 hours prior to collection and disposable.
5. A ‘Virtual first’ approach
We have a ‘virtual first’ approach where-by remote consultations remain standard practice during this period.
All initial contact and triage assessment to be conducted via remote means to establish:
- the risk a face-to-face appointment poses to the patient, those in the patient’s household, themselves, others in the clinical setting and the general public
- the clinical need of the patient
All decision making with appropriate rationale will be recorded in a patient’s clinical record.
6. Per patient risk assessment
We undertake per patient risk assessments and make a clinically reasoned decision for offering either a face-to-face or remote consultation for each patient and for each of their planned contacts. We document our rationale for these decisions.
Screening patients for face-to-face appointments will:
- minimize COVID-19 exposure and transmission
- ensure safety, in particular to those who belong in the clinically vulnerable and extremely clinically vulnerable groups
- allow for the support of urgent care needs when the risk of not seeing the patient and providing access to physiotherapy may lead to hospital admission or worsening of a condition
The clinicians decision to conduct a face-to-face or remote appointment must be based on whether the clinician can justify that the benefits of seeing a patient face-to-face are demonstrably greater than the risks of infection transmission.
The clinicians justification for conducting a face-to-face appointment must be documented in the clinical notes for each appointment.
7. Patient consent for treatment
We engage in discussions regarding the rationale for remote or face-to-face consultations with patients. Face-to-face consultations only occur if both parties deem it necessary to proceed with face-to-face care. The patient is made aware of all current risks associated with this approach and they provide written consent in advance of the face-to-face consultation.
Prior to the initial face-to-face session the patients’s are provided with the following information:
- the mechanisms and risks of transmission and exposure of covid-19
- the nature of close patient contact during a physiotherapy consultation
- the level of PPE that a clinician will be required to wear
- the infection prevention and control measures that must be taken by myself and the practitioner
Patients are required to provide written consent within 24 hours of their initial appointment to confirm they:
- Are not experiencing or have not experienced in the last 14 days any COVID-19-related symptoms.
- Have had not any contact with anyone with suspected or confirmed COVID-19 in the last 14 days.
- Have read and understood the Beyond Health Safeguarding Information
For each face-to-face session the clinician must also document in the patient’s clinical record that risks have been discussed and that the patient gives consent or not for treatment to proceed with a face-to-face consultation.
8. Staff Training
We demonstrate our duty of care as employers by ensuring all staff are trained and competent in the procedures necessary for the safeguarding of patients and employees during the covid-19 pandemic.
We follow the government guidance for employers.
Staff training is documented, signed by both trainer and trainee and filed with the clinic training records.
Staff training consists of:
- Review of the Beyond Health COVID-19 Safeguarding & Operational Policy and all associated guidelines
- Review and discussion with Manager of risk management assessment and mitigation strategies
- Operational walk-through of all new processes and procedures
Contact Us
We hope you find this information useful. If you’ve any question you can always call us at the clinic on 020 3848 9434 or send us an email at [email protected].

