
Close
Enquiry
Please see contact information below or complete the form and we will get in touch with you.

Parsons Green
3rd Floor Brigade House
8 Parsons Green
London
SW6 4TN
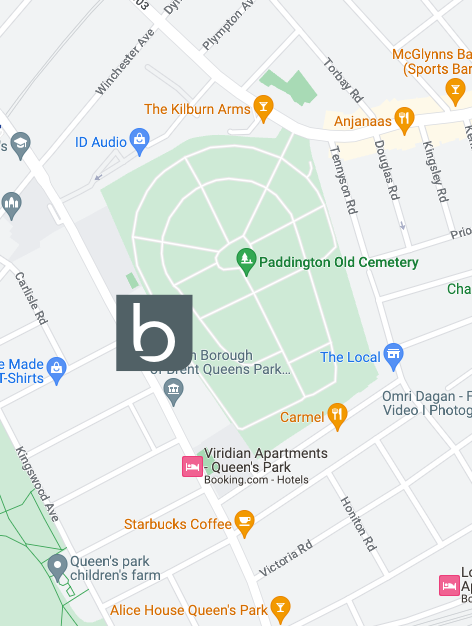
Queen's Park
2nd Floor
105-109 Salusbury Road
London
NW6 6RG

Jesse's House
8-10 Heathmans Road
Parsons Green
London
SW6 4TJ
Pelvic Health Physiotherapy – Part 2 of 4

Introducing Pelvic Health Physiotherapy (and everything you ever need to know about Pelvic Floor Dysfunction) – Part 2 of 4
As we explained in the first article of this series, Pelvic Health Physiotherapy is a specialist area within the field of musculoskeletal health that involves the non-surgical treatment of the pelvis and pelvic floor. To more accurately describe the nature of this specialist area the Chartered Society of Physiotherapy have recently changed the name of “Women’s Health Physiotherapy” to “POGP – Pelvic Obstetric and Gynaecological Physiotherapy”. In this the second of four “For Women Only” articles we explore in detail three specific Women’s Health conditions.
Pelvic Floor Dysfunction: Spotlight on Different Aspects
Menstruation, pregnancy and menopause can all lead to changes in oestrogen levels and a weakened pelvic floor, hence most women are at risk. The pelvic floor muscles will always be weakened during pregnancy and can be damaged during childbirth or stretched due to normal weight gain, but there are a range of other risk factors including;
- repeated strain associated with constipation or cough
- frequent heavy lifting
- regular high impact exercise
- obesity
- chronic back pain
- gynaecological surgery
- trauma to the pelvic region
- ageing
Here we discuss 3 specific Women’s Health disorders; Urinary Incontinence, Pelvic Girdle Pain, and Sexual Dysfunction.
1. Urinary Incontinence
Urinary Incontinence is very prevalent in the general population and therefore not an uncommon problem but this is NOT normal and you do not have to put up with this at times debilitating and embarrassing condition!
Here are some astonishing statistics:
- 40% of women over 40 years of age will suffer urinary incontinence (Medical Research Council)
- Between 20 – 60% of pregnant women and one third of new mothers will suffer from stress incontinence (Morkved et al 2003)
- In last trimester 48% of first time mothers and 85% of multiple pregnancy mothers will experience urinary incontinence (Morkved & Bo 2003)
- 92% of women who are incontinent 12 weeks after birth will still be at 5 years (Viktrup et al 2000)
- 5-7 years post-delivery 44.6% of women will have some degree of incontinence (Wilson et al 2002)
Why does it happen?
Incontinence can occur at any age but most commonly after giving birth or around menopause.
Changes in posture and in hormones lead to a weakening of the pelvic floor muscles resulting in insufficient support to the pelvic structure or the bladder. The extra weight and pressure of a pregnancy means that all pregnant women will have a weaker pelvic floor at the end of pregnancy than at the beginning. With stress incontinence, the bladder can’t cope with the pressure (stress) of a full bladder and leakage is experienced. Urge incontinence is surprisingly often not physical but psychological and/or habitual. Some individuals may have an immediate urge to go to the loo with specific triggers such as hearing running water.
What to do about it
Urinary incontinence and other pelvic floor dysfunction symptoms may require intervention. Wearing pads is absolutely NOT the answer for women with incontinence. There are a range of treatment options available to manage these responses. An assessment by a specialist pelvic health physiotherapist should be your first port of call.
2. Pelvic Girdle Pain (PGP) during pregnancy
PGP affects around 20% of women in pregnancy and is described as pain in either the pubic bone area, either or both sides of the groin or the sacroiliac joint. It can begin any time during pregnancy, during labour or post-delivery and does not always resolve after delivery.
This type of pain is described as very sharp, specific and usually on one side. If you have this pain you will notice it on activities where you partially separate your legs when walking stairs, standing on one leg to put trousers on and especially when turning in bed. This pain is eased with rest.
Why does it happen?
It is not clear why this occurs in some women and not others. The following elements are, however, known to be contributing factors:
- Pregnancy hormones relax ligaments which can cause a decrease in stability and an increased risk of pelvic pain
- Weight changes put added strain on bone and joints
- Postural changes due to centre of gravity changes
- Muscular changes such as the separation of your rectus muscle and the stretching and weakening of your core muscles means the pelvis has less support
What to do about it
PGP can be very frustrating and a double-edged sword because women will have been encouraged to exercise but this causes pain. If you are experiencing pain we suggest you try the following little things that can make a big difference:
- modify your activities
- keep your knees together when turning over in bed
- take smaller steps when walking
- sit down when putting trousers on
- try ice (a bag of frozen peas will do) on your pubic bone
If you have modified your activities but you are still experiencing pain then you will benefit from an assessment of your pelvic alignment.
3. Sexual Dysfunction
Some women can experience reduced sensation, awareness and control as a consequence of weakened pelvic floor muscles. Some women also experience pain.
Why does it happen?
While various physiological, anatomical and hormonal changes are thought to contribute to sexual dysfunction, a strong link between normal pelvic floor function and healthy sexual function has been shown.
Pelvic floor function can be impacted by pregnancy and surgical or hormonal interventions which can cause over-activity or weakening in these muscles.
What to do about it
Research suggests that reactivating and improving pelvic floor strength enhances sensation. Once again, many women may be embarrassed about discussing these challenges and suffer in silence. If some of these symptoms mentioned are of concern to you you can telephone the clinic and arrange for one of our Women’s Health Physiotherapists to contact you to discuss whether a consultation would be appropriate for you.
Next week in the third article of our “For Women Only” series we revisit client Jill’s question to one of our pelvic health Physiotherapists “Why is pelvic health Physiotherapy given so low a profile in the United Kingdom??”. We also provide some exercises to empower you to take the health of your pelvic floor into your own hands. Stay tuned!

